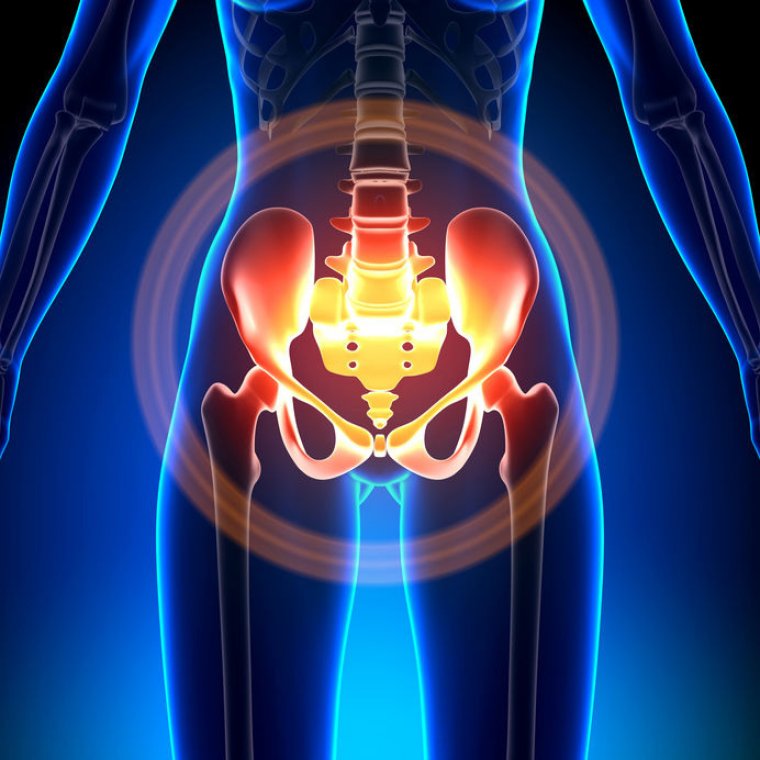
Taking Control Of Pelvic Pain: What is the pelvic floor? The pelvic floor is a group of muscles that form a hammock-like sling from the pubic bone to the tailbone. These muscles play an important role during urination, bowel movements and sexual intercourse. The pelvic floor coordinates with the diaphragm, abdominals and surrounding musculature to correctly contract and relax during these activities.
What causes pelvic floor pain? Many factors play a role in pelvic floor function.
Among them are:
- Posture
- Low back, pelvic and hip joint motion
- Muscle flexibility, strength and coordination
- Stress
- Psychosocial conditions
- Medical pathology
Dysfunction, arising from any combination of these factors, can lead to stress and strain in the pelvic floor and surrounding musculature. Repetitive stress and strain of these muscles over time can cause trigger points (taut bands/spasms within muscles) to develop in and around the pelvic floor, thus causing tension and pain. Trigger points can refer pain away from the original site of injury. Referred pain can lead to body compensations and create a vicious cycle of symptoms leading to abnormal posture and difficulty with daily tasks such as sitting, standing and walking. Tension can also lead to visceral symptoms (arising from the organs) such as difficulty with urination, urinary frequency, urinary and fecal incontinence, constipation, and painful intercourse. However, the opposite an also occur where organ problems can cause muscular pain that resists even after the original organ problem is resolved.
What are the symptoms of pelvic floor pain?
Pelvic pain can have many different characteristics such as:
- Dull, achy pain,
- Stabbing and cramping pain,
- Pain that is steady and non-remitting
- Pain that comes and goes
- Heaviness or congestion in the vaginal/ rectal region.
It is difficult for an individual and at times even physicians and physical therapists to know where pelvic pain is originating. It is very important to follow up with a specialist (i.e. urologist, gynecologist, gastroenterologist) to rule out medical pathologies before attempting to self —treat or have treatment performed on to the pelvic floor.
What can cause pelvic floor pain? Some medical conditions that can cause chronic pelvic pain are:
- Endometriosis
- Interstitial Cystitis,
- Fibroids
- Irritable Bowel Syndrome
- Pelvic Congestion Syndrome
- Pelvic Inflammatory Disease
- Ovarian Remnant
- Pelvic floor tension
How can a physical therapist help with my taking control of pelvic pain? A physical therapist can work in conjunction with your doctor to help alleviate and manage your pain associated with some of these medical conditions.
Many physicians are not yet aware or do not know therapists that can treat the pelvic floor as pelvic floor therapy has very recently gained popularity among the medical community. It may be beneficial to ask your physician if he or she feels physical therapy may be of benefit to your condition. Once you and your doctor have decided that seeking physical therapy treatment may be beneficial, it is also important to find a highly qualified physical therapist with good manual skills (hands-on skills) familiar with this patient population. Treatment requires a thorough evaluation of the musculoskeletal system including the low back, pelvis, hip and an internal pelvic floor exam to safely and correctly manage your symptoms. Often times a therapist will also perform a biofeedback exam to accompany the musculoskeletal evaluation. This latter exam is important but evaluation and treatment should not be limited to just biofeedback. Treatment limited to biofeedback may result in temporary relief but often times symptoms are more thoroughly and successfully managed with a thorough treatment of the musculoskeletal system and appropriate manual skills to treat the trigger points causing pain. Treatment can include postural correction, education and awareness, improving joint motion and stability, increasing muscle strength and flexibility and coordination training, and trigger point release of the pelvic floor and surround soft tissue.
What can I do before starting physical therapy treatment to take control of my pelvic pain?
Diaphragmatic Breathing and why is it important to decrease pelvic pain. The diaphragm is a sheet of muscle that spans across the bottom of the rib cage and is the primary muscle used for breathing. Diaphragmatic Breathing or full deep breathing is a way of breathing in which you engage the diaphragm and allow the abdominals to expand. It is the key to decreasing muscle tension and improving coordination. Because of modern-day stresses, increased activity of the sympathetic nervous system (part of the nervous system activated during stress) and the idea of having flat/tight abdominals, individuals have little awareness and difficulty engaging their diaphragms. Excess tension in the belly creates increased tension in the chest, low back, and pelvic floor muscles leading to pain. Many Individuals with chronic pelvic pain use increased muscle effort and have difficulty performing this breathing simultaneously with a kegel/ pelvic floor contraction (contraction used when you hold back urine). The ability to perform these two exercises together is a key component to improving pelvic floor coordination, increasing flexibility and reducing pelvic pain.
How to Diaphragmatically Breathe Start in a quiet environment where you can concentrate on your breathing. Closing the eyes can facilitate this concentration. Start in a laying down position and place one hand on the belly and one hand on the chest. As you breathe in, allow your belly to expand as much as it can but keep your chest still. Try and make these breaths long, drawing air into the lungs slowly. As you breathe in your belly should rise. As you breathe out your belly should fall. At first, this breathing may seem difficult and awkward to perform. With concentration and practice, this will become easier to perform and will become your primary way of breathing. Once you are able to perform this with ease, try and perform this breathing in sitting, standing and daily activities. Once you have mastered this, you are ready to move to the next step.
Diaphragmatic Breathing with a Pelvic Floor Contraction/ Relaxation Now that you are comfortable with performing diaphragmatic breathing, it is time to try and coordinate this with your pelvic floor muscles. Start in a laying down position with one hand on the belly and the other on the chest. As you breathe in, try and fully relax your pelvic floor muscles (as if you are trying to initiate urination). As you breathe out, contract your pelvic floor muscles (as if you are trying to hold back urine). Try and perform these slowly with control. Once you are able to perform this with ease and without holding your breath, you should try and incorporate this during sitting and standing.
Diaphragmatic Breathing with Use of Dilators I only recommend performing the following exercises once you have been instructed by an appropriate health care professional in the proper use of dilators.
Dilators are rod-like tools that are usually made of smooth rubber or plastic that can help improve vaginal elasticity. When the pelvic floor muscles are tight, they need to be stretched just like someone with a tight hamstring needs to stretch. Dilators help stretch the pelvic floor muscles and also help stretch any scar that has developed from other injuries and medical procedures (i.e. vaginal tearing/ episiotomy from a delivery).
Dilators usually come in several graduated sizes. Start with the smallest one that can be used comfortably. Start by making sure your dilator has been thoroughly cleaned with soap and water. (Remember certain detergents can irritate the skin).
Apply a water-based lubricant such as KY Jelly or Fem Glide on the dilator and a small amount near the vaginal opening. Lay on your back with your knees bent and legs spread apart. Gently insert the dilator into the vagina (with gentle pressure but not with force) while trying to remain as relaxed as you can and performing diaphragmatic breathing:
Try and hold the dilator in place for 10-15 minutes while continuing to breathe. Once you can perform this with minimal discomfort over a few weeks you can try to move the dilator in and out and rotate it while performing diaphragmatic breathing. If you come to a painful spot (a possible trigger point) you can try to apply gentle pressure or sweep the dilator back and forth across the spot for a few seconds. Make sure you are not hitting the pubic bone.
Once you can use the smaller dilator with minimal discomfort you are ready to try the next size. Initially start by using the smaller dilator for 5 minutes and then use the larger size for 5 minutes. End with using the smaller one again for another five minutes.
Frequency Dilators should be used daily until you have reached and are able to use the satisfactory dilator size for about 1 month (usually the size that allows you to successfully use a tampon or have intercourse with minimal discomfort). You can decrease the frequency to every other day for 2-6 months and then 2-3 times per week to maintain vaginal flexibility.
THIS TIP WAS WRITTEN BY Hina Sheth MPT, OCS, MTC A PHYSICAL THERAPIST IN PHILADELPHIA
